This blog charts my experience on anticogulants, as a 32 year old in the UK, after having heart surgery to replace a faulty Aortic Valve.
I will attempt to share my knowledge in the hope that it will help other patients, something I could have found very useful.
This exposes the mess that our healthcare system has got itself into in the UK and shows some of the misinformation spread by health professionals about the drug.
Monday, 31 December 2012
Monday, 9 July 2012
Calorific Intake Affect on Warfarin
I've talked before about the relationship with my calorie intake and warfarin, and here are some more conclusions and a time line.
Anyone that has ever tried to go on a calorie controlled diet will know that it inevitably becomes a low carb diet. It's almost impossible to fill your stomach and feel satisfied with food by eating carbs, so you end up eating more veg and meat.
Here is a rough timescale of how my dieting went this year, and how it affected the INR:
The whole of 2012: My average dose was 7.6mg
2012 up to January 12th: My average dose was 8.5mg
--Diet starts on January 12th. Calorie controlled, nutritionally balanced diet, low carb--
Jan 12th - Jan 31st: My average dose was 9.5mg
Throughout February: My average dose was 10.1mg
--Diet "back to normal" - eating whatever takes my fancy.
Throughout March: My average dose was 10.9mg
Throughout April: My average dose was 9.2mg
Throughout May: My average dose was 9.0mg
Throughout June: My average dose was 8.6mg
--Diet starts again... time to reduce weight a little--
I have now proactively increased my dose to anticipate a higher dose requirement on the lower calorie diet.
My conclusion of the above: Dieting in this manner has a medium-term effect on the way your liver deals with the warfarin. The dose slowly rises during the diet (over a month or two) and then slowly goes back down after you end the diet (over 3 months).
This shows just how much diet can change your dosing, and how important it is not to consider that you simply have "my average". This average can change over time.
This is further reinforcement that a self-tester should be testing regularly, and using as much knowledge as they can to anticipate correct dosing.
Anyone that has ever tried to go on a calorie controlled diet will know that it inevitably becomes a low carb diet. It's almost impossible to fill your stomach and feel satisfied with food by eating carbs, so you end up eating more veg and meat.
Here is a rough timescale of how my dieting went this year, and how it affected the INR:
The whole of 2012: My average dose was 7.6mg
2012 up to January 12th: My average dose was 8.5mg
--Diet starts on January 12th. Calorie controlled, nutritionally balanced diet, low carb--
Jan 12th - Jan 31st: My average dose was 9.5mg
Throughout February: My average dose was 10.1mg
--Diet "back to normal" - eating whatever takes my fancy.
Throughout March: My average dose was 10.9mg
Throughout April: My average dose was 9.2mg
Throughout May: My average dose was 9.0mg
Throughout June: My average dose was 8.6mg
--Diet starts again... time to reduce weight a little--
I have now proactively increased my dose to anticipate a higher dose requirement on the lower calorie diet.
My conclusion of the above: Dieting in this manner has a medium-term effect on the way your liver deals with the warfarin. The dose slowly rises during the diet (over a month or two) and then slowly goes back down after you end the diet (over 3 months).
This shows just how much diet can change your dosing, and how important it is not to consider that you simply have "my average". This average can change over time.
This is further reinforcement that a self-tester should be testing regularly, and using as much knowledge as they can to anticipate correct dosing.
May 29 2012 - Holiday in Venice
For this holiday I drank zero alcohol, i wanted to see if it was a factor on my usual holiday INR Highs!
For anyone that has visited Venice you will know that you spend the whole day walking. Fair enough, but tiring. On the first day, after 12 hours of walking, my muscles were aching and I was feeling tired. We pushed on, and then I got a sudden stabbing pain in my foot. I literally could not walk, and it got worse and worse as I limped home.
This was still hurting like crazy 5 days later.
Warfarin related? Who knows - but i think so. Some form of a bleed in my foot caused by excessive exercise.
Why was the INR high? Equally - I don't know. Stress of Travel? Altered Diet? Maybe.
This kind of thing still randomly happens sometimes:
I had a 45 minute phone call with my GP's partner. Not my original GP I might note. She had a totally different attitude to him, and was happy to sponsor my own self testing and dosing.
She explained that not everyone was suited to it like myself, and apologised for the hassles the old system offered.
I now have PT Test Strips on Prescription as required for testing every 2 days.
In return so she can ensure I am operating safely, I have to submit a print out of my Warfarin diary every month, and go for a full blood test every 6 months. (Not another finger-prick test i might add).
What a total victory!!
March 2nd 2012. Fed Up.
I finally got totally fed up with having to go to the pharmacy for tests and decided to write some strong letters to the pharmacy, the GP, my cardiologist and the head of clinical services. I'm taking exception with the fact they ignore my own results and then make incorrect dosing decisions based on a single snapshot test.
Here's my letter:
Dear Dr. XXXX,
I wanted to write this letter to let you know my situation, and intentions in regard to my Anticoagulant therapy.
I have in fact been self-testing and self-dosing for coming up to a year. I adjust my own dose regularly to take into account lifestyle changes, and I do not inform the pharmacy of these changes. I have bi-daily records of tests and daily doses for every single day since therapy started, and statistics that show a very successful INR in-target for this time. I have carefully researched Warfarin management across the world, and across the UK, and believe that my Warfarin is managed better than could ever be achieved through spot checking. I am part of the Oxford University CASM Anti-coagulant self-monitoring study group, and take an active part in discussions with other Warfarin self-testers across the world through the internet. I note that the original concept of bi-daily testing and self-management came from my Heart Surgeon who I quite literally trusted with my life and will follow his advice to self manage Warfarin.
My intention is to officially be recognised as self-managing my Warfarin, something that is happening across the UK and already yielding fantastic results. I have a friend in Wales who does this, and another in Essex - I attach the NHS Policy from the Essex area which I would be delighted to follow. I am looking to visit a health professional for testing no more than every 6 months. Note that whether officially recognised as self-managing or not, I will continue to do so regardless, but I believe it is in every ones interest for honesty and openness and working together for the best results.
I recently missed several appointments and was chased up as if my life were in danger, with no recognition that I self test - and then my Warfarin was withheld unless I took a test. I question the legality of this, as withholding the drug from me puts my life in jeopardy. I now have 2 months supply of tests and Warfarin and hope that I can resolve the situation in this time, as I have no intention of attending any further appointments.
As an active 33 year old on Warfarin for the rest of my life it is critically important to me to resolve this situation and free me from the constant chore of visiting the pharmacy for tests that serve no practical purpose other than to follow a published policy. It is causing me considerable stress and causing problems with my working hours. My intent is to officially establish my position of a warfarin self manager, and I am now embarking on a letter campaign to make this become a reality.
I have also written a very similar letter to XXXX at XXXX (Pharnacy) and Dr.XXXX (Medical Director of the NHS Trust, and my Cardiologist).
Kind Regards,
-Carl.
February 21st 2012. Head Injury
I was working on my kitchen extension - not really doing anything important, just sweeping up. I had no protection on because I wasn't doing much... but of course, that's when it gets you!
A concrete block fell from a height of 7 feet high, bounced off the wall, and the corner hit me on the head, a glancing blow. I was squatting, and it threw me off my feet back onto my behind. I immediately held my hand to my head, and it was covered in blood.
My girlfriend rushed me to A&E, and she was talking to me the whole time to check I remained conscious and not concussed. I was still losing blood, it was running down my face, but it was clotting up and matting my hair.
I waited for the doctors to see me - not long at all - because of the Warfarin i was high on the list and went past many others. It had stopped bleeding by the time they saw me, so they super-glued it back together - i had a half inch gash on top right of my head.
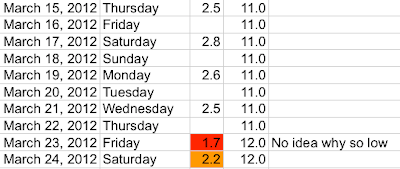
Here are my INR results... I think I was lucky it was low! Not sure that a 3.5 would have been so kind to me.
Anyway, I recovered fully, obviously, with no futher negative effects. However, I was carefully monitoring myself for the week after.
A concrete block fell from a height of 7 feet high, bounced off the wall, and the corner hit me on the head, a glancing blow. I was squatting, and it threw me off my feet back onto my behind. I immediately held my hand to my head, and it was covered in blood.
My girlfriend rushed me to A&E, and she was talking to me the whole time to check I remained conscious and not concussed. I was still losing blood, it was running down my face, but it was clotting up and matting my hair.
I waited for the doctors to see me - not long at all - because of the Warfarin i was high on the list and went past many others. It had stopped bleeding by the time they saw me, so they super-glued it back together - i had a half inch gash on top right of my head.
Here are my INR results... I think I was lucky it was low! Not sure that a 3.5 would have been so kind to me.
Anyway, I recovered fully, obviously, with no futher negative effects. However, I was carefully monitoring myself for the week after.
Not written for a while
I realised I haven't posted on here for quite a while - thanks to Jeff for reminding me. I think I generally feel that i've posted everything there is to say, and the topic doesn't change much. From here I expect to only learn small new things, not much changes day-to-day. However, I'll make a couple of postings now with reference to my Diary... there are always a few mini-surprises in there!
Monday, 16 January 2012
Can I Drink Alcohol when i'm on warfarin?
I've received several emails from people, all with the same theme - "Can I still go out and have a few drinks when I'm on Warfarin". My answer is ….
Thanks for asking the question, this is really the whole point of my blog and the reason I want to post the information online. Its about living the life you want to live and not feeling restricted by the drug. Unfortunately I've spent more effort defending myself from the older folks, the ones with the compatively boring and stable lives than I have answering this very question.
I built up to my alcohol research, i didn't just go and get smashed. I had heard the horror stories of alcoholics and people who just didn't care. So, I tried a glass of wine, and tested INR. No effect. Then 2 glasses… no effect. Then 3 … still no real effect, perhaps a tiny one. Everybody's different, particularly the old folks, but everyone needs a different dose of warfarin to maintain their level, so perhaps alcohol has different effects on different people.
In the 7 months since my operation I've had plenty to drink. I enjoy wine at home several nights a week, and at the weekend often go out and have quite a few. A typical friday night might be 2 beers, half a bottle of wine, and another beer for the road, or something like that. I've never found this level of drinking to cause a problem.
In that time i've got drunk 3 times. My definition of drunk is that I'm still walking, I haven't vomited, but i'm pretty much mentally gone. These have been single binge drink sessions. On each occasion, the warfarin raised a little - nothing even alarming. I always knew that the INR was in range before I set out drinking, that's the nice thing about testing so regularly. In most cases the INR was something like 2.7 and raised up to 3.0. Whenever I know I was going out drinking - a party, or friday night, i could can cut the warfarin dose just a little for the 2 days before. Obviously don't do this if you're already running a bit low. To be honest, the dosing is common sense. Don't be scared of changing the dose, it's a slow reacting drug and you can chop your dose all over the place and the difference it makes is pretty small.
One problem of course is that alcohol can lead to people being clumsy, aggressive, etc... and these things could mean you're more likely to fall over or get into a fight. I can't help you in this area! Suffice to say it's not a good idea, blunt force trauma can cause some pretty nasty things to happen to your body, you should consider yourself to be a bit more fragile when on warfarin, particularly if your INR is high. In my opinion if you don't know what your INR is, if you haven't tested for more than 3 days, then you should consider the worst case. Make sure you test every 3 days, minimum.
Drinking several days in a row has more of an affect, and this requires more management. The attached little picture was the stats of going on christmas holiday with a friend. I was out drinking every night… usually just a couple of beers each day, but on one day half a bottle of wine too. It required management to kerb the rising INR - unfortunately on this case I was also on cold meds which include paracetomol, so i got the double wammy. Its a shame I don't have enough scientific information about just drinking alone, this was my first multiple-day drinking session since the operation. As you can tell from reading the blog, this all went very badly - the combination of alcohol, cold meds, and hurting my arm left me with a month of pain. I still don't really know how much of that was cold meds versus alcohol, but I suspect a bit of both. The INR climbing so high on alcohol alone doesn't sound possible to me, when I look at my other results from previous drinking.
So in summary, i would never give a blanket answer to just go out and drink, instead I say that you should test very regularly, even daily after an "event" that might damage your stability such as drinking. If you're totally on top of the situation, you can then experiment with how much drinking you can do personally…. for me, it's not been a problem.
There's half a chance if you're reading this that you are about to have a heart valve replaced, like me. You are weighing up the Bio/Pig/Cow valve against the mechanical. The answer is a no-brainer - mechanical every time. Anyone under the age of 50 would be an idiot to go with a Bio valve no matter what the perceived benefit. You will become a ticking time bomb just waiting for the valve to fail and require a re-op - i couldn't live with that. The only downside of the mechanical valve is the warfarin, and it's really no problem at all. It's easier than diabetes and slightly harder than taking a birth control pill. No biggie. The only other downside for mechanical valves that I considered at the time was the ticking noise.... well, Same answer again, with my On-X it's so quiet that nobody has ever heard it without me shoving their ear against my chest, and I don't hear it any more at all - I heard it a little at first, but it was kind of pleasant and never stopped me sleeping.

Thanks for asking the question, this is really the whole point of my blog and the reason I want to post the information online. Its about living the life you want to live and not feeling restricted by the drug. Unfortunately I've spent more effort defending myself from the older folks, the ones with the compatively boring and stable lives than I have answering this very question.
I built up to my alcohol research, i didn't just go and get smashed. I had heard the horror stories of alcoholics and people who just didn't care. So, I tried a glass of wine, and tested INR. No effect. Then 2 glasses… no effect. Then 3 … still no real effect, perhaps a tiny one. Everybody's different, particularly the old folks, but everyone needs a different dose of warfarin to maintain their level, so perhaps alcohol has different effects on different people.
In the 7 months since my operation I've had plenty to drink. I enjoy wine at home several nights a week, and at the weekend often go out and have quite a few. A typical friday night might be 2 beers, half a bottle of wine, and another beer for the road, or something like that. I've never found this level of drinking to cause a problem.
In that time i've got drunk 3 times. My definition of drunk is that I'm still walking, I haven't vomited, but i'm pretty much mentally gone. These have been single binge drink sessions. On each occasion, the warfarin raised a little - nothing even alarming. I always knew that the INR was in range before I set out drinking, that's the nice thing about testing so regularly. In most cases the INR was something like 2.7 and raised up to 3.0. Whenever I know I was going out drinking - a party, or friday night, i could can cut the warfarin dose just a little for the 2 days before. Obviously don't do this if you're already running a bit low. To be honest, the dosing is common sense. Don't be scared of changing the dose, it's a slow reacting drug and you can chop your dose all over the place and the difference it makes is pretty small.
One problem of course is that alcohol can lead to people being clumsy, aggressive, etc... and these things could mean you're more likely to fall over or get into a fight. I can't help you in this area! Suffice to say it's not a good idea, blunt force trauma can cause some pretty nasty things to happen to your body, you should consider yourself to be a bit more fragile when on warfarin, particularly if your INR is high. In my opinion if you don't know what your INR is, if you haven't tested for more than 3 days, then you should consider the worst case. Make sure you test every 3 days, minimum.
Drinking several days in a row has more of an affect, and this requires more management. The attached little picture was the stats of going on christmas holiday with a friend. I was out drinking every night… usually just a couple of beers each day, but on one day half a bottle of wine too. It required management to kerb the rising INR - unfortunately on this case I was also on cold meds which include paracetomol, so i got the double wammy. Its a shame I don't have enough scientific information about just drinking alone, this was my first multiple-day drinking session since the operation. As you can tell from reading the blog, this all went very badly - the combination of alcohol, cold meds, and hurting my arm left me with a month of pain. I still don't really know how much of that was cold meds versus alcohol, but I suspect a bit of both. The INR climbing so high on alcohol alone doesn't sound possible to me, when I look at my other results from previous drinking.
So in summary, i would never give a blanket answer to just go out and drink, instead I say that you should test very regularly, even daily after an "event" that might damage your stability such as drinking. If you're totally on top of the situation, you can then experiment with how much drinking you can do personally…. for me, it's not been a problem.
There's half a chance if you're reading this that you are about to have a heart valve replaced, like me. You are weighing up the Bio/Pig/Cow valve against the mechanical. The answer is a no-brainer - mechanical every time. Anyone under the age of 50 would be an idiot to go with a Bio valve no matter what the perceived benefit. You will become a ticking time bomb just waiting for the valve to fail and require a re-op - i couldn't live with that. The only downside of the mechanical valve is the warfarin, and it's really no problem at all. It's easier than diabetes and slightly harder than taking a birth control pill. No biggie. The only other downside for mechanical valves that I considered at the time was the ticking noise.... well, Same answer again, with my On-X it's so quiet that nobody has ever heard it without me shoving their ear against my chest, and I don't hear it any more at all - I heard it a little at first, but it was kind of pleasant and never stopped me sleeping.

Well I'm back home from holiday now, have been a few days, and my arm is just about better…. I have full movement. There is still a little tenderness in the muscle.
Unfortunately there is STILL bruising showing... see the picture below!
It's now 1 month since the "injury" occurred. This is an amazingly long time for the blood to drain.
Unfortunately there is STILL bruising showing... see the picture below!
It's now 1 month since the "injury" occurred. This is an amazingly long time for the blood to drain.
Thursday, 5 January 2012
Following comments on valvereplacement.org, here I have posted the following further information:
Thanks for taking the time to read and comment.
I knew it would be controversial, particularly the frequency of testing.
The reason I chose to test so frequently was really to challenge the incumbent beliefs about stability and to try and uncover the truth of what the INR level does on a more regular basis.
I agree that if the typical dosage calculators are followed then it would cause yo-yo effect, and that's because the calculators only ever look at a single dose. My strategy is different - i look at the range of doses and INRs over the last few days and look for a trend. I then make a dose change to arrest that change…. or often just don't bother.
My time on the drug so far has seem some very successful dosing and small dose adjustments, and it's also seen some mistakes. I will keep refining this.
I'm a software developer by trade and i'm working on a new algorithm calculator tool that will support my dosing. It's a very complex algorithm so I haven't managed to create it yet, but it's definitely on the way. It will look at a whole week's results and doses before making a dose suggestion.
I believe that the "perfect" system would be to test every single day, and to change the dosage daily making small adjustments to arrest any trend up and down. I this were followed I believe warfarin would be in range for an even higher percentage of the time.
I will continue to test very regularly and keep refining my method. Certainly regular testing doesn't do any harm, it gives a great insight into what's actually going on.
Remember that all of this is based on my statistical interest, and on the fact I don't believe warfarin to be a stable drug. Not a mainline opinion, but certainly mine.
Thanks for taking the time to read and comment.
I knew it would be controversial, particularly the frequency of testing.
The reason I chose to test so frequently was really to challenge the incumbent beliefs about stability and to try and uncover the truth of what the INR level does on a more regular basis.
I agree that if the typical dosage calculators are followed then it would cause yo-yo effect, and that's because the calculators only ever look at a single dose. My strategy is different - i look at the range of doses and INRs over the last few days and look for a trend. I then make a dose change to arrest that change…. or often just don't bother.
My time on the drug so far has seem some very successful dosing and small dose adjustments, and it's also seen some mistakes. I will keep refining this.
I'm a software developer by trade and i'm working on a new algorithm calculator tool that will support my dosing. It's a very complex algorithm so I haven't managed to create it yet, but it's definitely on the way. It will look at a whole week's results and doses before making a dose suggestion.
I believe that the "perfect" system would be to test every single day, and to change the dosage daily making small adjustments to arrest any trend up and down. I this were followed I believe warfarin would be in range for an even higher percentage of the time.
I will continue to test very regularly and keep refining my method. Certainly regular testing doesn't do any harm, it gives a great insight into what's actually going on.
Remember that all of this is based on my statistical interest, and on the fact I don't believe warfarin to be a stable drug. Not a mainline opinion, but certainly mine.
Wednesday, 4 January 2012
2011 - Statistics
I keep every single test and result in a spreadsheet, and compile statistics from it. For the year, my statistics are detailed below.
In summary:
I took 241 doses over 34 weeks. In this time I tested 159 times. That's an average of testing every 1.5 days.
My average result was 2.75 which is ridiculously perfect! I was out of range plenty of times and actually only in range 53% of the time. Interestingly i was out of range positively almost exactly as many times as negatively. My lowest reading was 1.7 and highest 4.1. Not too bad I think.
My average dose was 7.61 which ranged from 4 to 12mg on a single 24 hour period. 8mg was my most commonly taken dose.
In summary:
I took 241 doses over 34 weeks. In this time I tested 159 times. That's an average of testing every 1.5 days.
My average result was 2.75 which is ridiculously perfect! I was out of range plenty of times and actually only in range 53% of the time. Interestingly i was out of range positively almost exactly as many times as negatively. My lowest reading was 1.7 and highest 4.1. Not too bad I think.
My average dose was 7.61 which ranged from 4 to 12mg on a single 24 hour period. 8mg was my most commonly taken dose.
DIY - Cutting myself!
I've always been into DIY, using lots of tools, and generally cutting and scratching myself regularly. I'm typically male in my attitude, i just ignore it, and if it's making a mess wrap it in whatever is handy, usually some sellotape or something!
Well, I can report that after being on warfarin, Nothing has changed here. Nothing. Heals the same, bleeds the same.
Banging myself however, different story. I definitely bruise easier, and it's noticeably worse when INR is up near 4.0.
Well, I can report that after being on warfarin, Nothing has changed here. Nothing. Heals the same, bleeds the same.
Banging myself however, different story. I definitely bruise easier, and it's noticeably worse when INR is up near 4.0.
Alcohol
Having been on warfarin for 8 months and had plenty of binge drinks, including week-long ones, i believe you can drink anything you want as long as you test regularly and alter the dose to suit.
Simple as that. Doctors don't want to hear it, but you really can drink whatever, whenever, as long as you test whenever your stability is at risk.
Simple as that. Doctors don't want to hear it, but you really can drink whatever, whenever, as long as you test whenever your stability is at risk.
NHS Advice Nonsense
NHS Advice on Warfarin isn't that far away from other worldwide advice, however, elements of it are not correct.
Particularly: "If you miss a dose, just skip it and take the next one as usual".
What a load of rubbish. If you do this you are guaranteeing yourself a dive in INR. I say instead "If you miss a dose, take it next morning." If you've already got around to the next day's dose, just take 150% of usual dose instead. At least this way you're attempting to stop the trend and get on top of it.
In addition the dosing algorithms are too general and not specific enough. I believe you can get on top of a high/low problem by looking at trend, history, and working out what makes sense. This of course requires regular testing, and the algorithms all assume you're tested very rarely indeed.
In summary: A decision cannot be correctly made on a single test snapshot, you require a number of test results to spot trends and patterns.
Particularly: "If you miss a dose, just skip it and take the next one as usual".
What a load of rubbish. If you do this you are guaranteeing yourself a dive in INR. I say instead "If you miss a dose, take it next morning." If you've already got around to the next day's dose, just take 150% of usual dose instead. At least this way you're attempting to stop the trend and get on top of it.
In addition the dosing algorithms are too general and not specific enough. I believe you can get on top of a high/low problem by looking at trend, history, and working out what makes sense. This of course requires regular testing, and the algorithms all assume you're tested very rarely indeed.
In summary: A decision cannot be correctly made on a single test snapshot, you require a number of test results to spot trends and patterns.
2012 Learnings - Warfarin Stability
Its January 2012 and I've just finished writing up all the diary history on this blog. I'm now going to write about my findings, conclusions and recommendations to date.
My overall summary is that I believe healthcare professionals approach the drug in entirely the wrong manner. The assumption is that warfarin is a stable drug and once you are "stable", the dose pretty much stays the same, although you might periodically adjust to deal with lifestyle changes. As long as you do everything consistently, it will be fine. And if it goes a bit high, they just blame you for not eating enough vegetables.
In my opinion this is completely wrong. I believe it's an unstable drug that goes through brief periods of apparent stability before finding the next reason to bite you. Its a reactive drug that has a million variables and a million drugs that interact with it. Nearly everything you do is affecting it in one way or another.
However, I can see why professionals would have come to this opinion. A typical patient might only get tested every few weeks, and that's enough time for it to be stable, go unstable, then stable again. So both test results will show around the same, and therefore the patient is stable. If they happen to have been badly low or high at any time in the period, nobody would have known.
Or perhaps they know this... and that's why they say "If you ever suffer bleeding come and see us". This very reactive approach to medicine is terrible, and extremely old fashioned. In this modern world with the technology we have, this just isn't acceptable. Notice how there's no offering in here for if it goes low... perhaps they should say "If you have a stroke, come see us too". Of course this doesn't apply to most warfarin patients to quite the level it does to a heart valve patient, but nobody wants clots floating around their body, they never do any good. So by the grace of god go all patients on warfarin, essentially crossing their fingers that the drug stays in order for most of the time.
Clearly I'm a huge self-test advocate, and one of many, but a very small minority in the overall warfarin population. There can only be two reasons against self testing - (1) that the typical elderly person can't do the test, too complex and fiddly and (2) costs. I think the elderly issue can be worked around, carers, family, etc - even if just testing weekly it would be an improvement. And costs - well, no answer here - they cost a fortune to run, so I suspect this is the real reason.
The most stupid thing out there is the attitude of the professionals towards me - I've seen a variety of attitudes towards self testing. Dismissive is the first one, a feeling that a patient couldn't possibly do anything themselves. Patronising follows closely after that one, why on earth would a patient want to self test. Next comes the bossy one, telling me not to test and not to dose.
The UK needs to update the rules to allow me to self-test and self-dose, then I could be honest with the professionals and work together with them instead of having to do it covertly.
My overall summary is that I believe healthcare professionals approach the drug in entirely the wrong manner. The assumption is that warfarin is a stable drug and once you are "stable", the dose pretty much stays the same, although you might periodically adjust to deal with lifestyle changes. As long as you do everything consistently, it will be fine. And if it goes a bit high, they just blame you for not eating enough vegetables.
In my opinion this is completely wrong. I believe it's an unstable drug that goes through brief periods of apparent stability before finding the next reason to bite you. Its a reactive drug that has a million variables and a million drugs that interact with it. Nearly everything you do is affecting it in one way or another.
However, I can see why professionals would have come to this opinion. A typical patient might only get tested every few weeks, and that's enough time for it to be stable, go unstable, then stable again. So both test results will show around the same, and therefore the patient is stable. If they happen to have been badly low or high at any time in the period, nobody would have known.
Or perhaps they know this... and that's why they say "If you ever suffer bleeding come and see us". This very reactive approach to medicine is terrible, and extremely old fashioned. In this modern world with the technology we have, this just isn't acceptable. Notice how there's no offering in here for if it goes low... perhaps they should say "If you have a stroke, come see us too". Of course this doesn't apply to most warfarin patients to quite the level it does to a heart valve patient, but nobody wants clots floating around their body, they never do any good. So by the grace of god go all patients on warfarin, essentially crossing their fingers that the drug stays in order for most of the time.
Clearly I'm a huge self-test advocate, and one of many, but a very small minority in the overall warfarin population. There can only be two reasons against self testing - (1) that the typical elderly person can't do the test, too complex and fiddly and (2) costs. I think the elderly issue can be worked around, carers, family, etc - even if just testing weekly it would be an improvement. And costs - well, no answer here - they cost a fortune to run, so I suspect this is the real reason.
The most stupid thing out there is the attitude of the professionals towards me - I've seen a variety of attitudes towards self testing. Dismissive is the first one, a feeling that a patient couldn't possibly do anything themselves. Patronising follows closely after that one, why on earth would a patient want to self test. Next comes the bossy one, telling me not to test and not to dose.
The UK needs to update the rules to allow me to self-test and self-dose, then I could be honest with the professionals and work together with them instead of having to do it covertly.
Subscribe to:
Comments (Atom)